 In recent years, public health authorities have expressed serious concerns regarding what they call the trend of “emerging infections.” They fear that many diseases transmitted by various pests—collectively called “vectors”— are on the rise. Even diseases eradicated from the United States are reemerging as increased travel and trade create more opportunities for diseases to cross international boundaries. Even diseases that have never been seen in the United States have emerged, such as the West Nile virus in 1999. In the past, we have been able to keep these diseases at bay with the use of pesticides and other measures, but today government regulations limit access to much-needed pesticides. In addition, environmental activists have waged attack campaigns on pesticide use, scaring the public about the risks of pesticides and failing to inform them of the far more serious risks associated with disease vectors. As a result, individuals and public health agencies have fewer options to control serious and expanding risks associated with vector-borne diseases.
In recent years, public health authorities have expressed serious concerns regarding what they call the trend of “emerging infections.” They fear that many diseases transmitted by various pests—collectively called “vectors”— are on the rise. Even diseases eradicated from the United States are reemerging as increased travel and trade create more opportunities for diseases to cross international boundaries. Even diseases that have never been seen in the United States have emerged, such as the West Nile virus in 1999. In the past, we have been able to keep these diseases at bay with the use of pesticides and other measures, but today government regulations limit access to much-needed pesticides. In addition, environmental activists have waged attack campaigns on pesticide use, scaring the public about the risks of pesticides and failing to inform them of the far more serious risks associated with disease vectors. As a result, individuals and public health agencies have fewer options to control serious and expanding risks associated with vector-borne diseases.
Background
Throughout history, one of the most serious risks to public health has been disease transmitted by vectors. Vectors include any organism that carries pathogens that can then be transferred to humans. Most commonly we think of mosquitoes and other insects, but rodents and other animals can transmit disease as well. We should learn from history that vector-borne risks are not isolated to tropical areas and that they can reemerge in the United States. Consider a few historical cases:
- In the summer of 1793, an epidemic of yellow fever, a disease carried by mosquitoes, struck Philadelphia. Yellow fever killed 5,500 people that summer and plagued the city for seven years.(1) Malaria was endemic in most of the United States and remained so in many states until right after the end of World War II.(2)
- Dengue fever periodically emerged the U.S. Gulf Coast states for decades including recent outbreaks in the 1980s, and it continues to pose a threat.(3) Tick-borne diseases have affected the population as well.(4)
- The research of Paul Reiter, chief of the entomology section of the Dengue Branch of the Centers for Disease Control and Prevention (CDC), demonstrates that, contrary to popular wisdom, most mosquito-borne diseases are not tropical. For example, he notes that until modern times, malaria was endemic in nearly all states east of the Rockies, as well as in Canada, Norway, Sweden, and northern Russia.(5)
Adverse Impacts of Vector-Borne Disease Today
 In the United States, Lyme disease is the number one vector-borne disease. Vector-borne diseases continue to plague the world. The developing world suffers the greatest toll because many nations cannot afford pesticides and other control methods. Consider these facts:
In the United States, Lyme disease is the number one vector-borne disease. Vector-borne diseases continue to plague the world. The developing world suffers the greatest toll because many nations cannot afford pesticides and other control methods. Consider these facts:
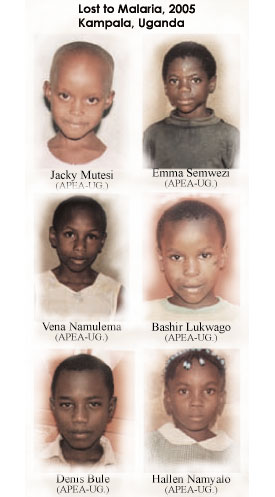
- According to the World Health Organization, malaria alone infects 500 million and kills more than 1 million.(6) Most of its victims are children.According to the CDC, “During 1992–1998, a total of 88,967 cases of Lyme disease were reported by 49 states, the District of Columbia, and Guam (2 cases), for a crude mean annual incidence of 5.1 reported cases/100,000 persons/year. The number of reported cases increased 70%, from 9,909 in 1992 to 16,802 in 1998. Ninety-two percent of cases were reported by 10 states. Over the 7-year period, crude annual incidence per 100,000 persons increased from 4.0 to 6.7.”(7) The CDC notes that reported cases have increased probably because of both better surveillance and true increases of incidence. Still, the CDC believes overall incidence is underreported, noting that more intensive studies in both Maryland and Connecticut find that there are 7 to 17 unreported cases for each reported case.
- In 1999, the West Nile virus appeared in the United States for the first time. Since then, it has killed hundreds of people and made thousands seriously ill.(8) The illness can be severe, leading to months of suffering and paralysis for some. The CDC estimates that thousands of cases were probably never reported.
- Vectors also promote serious problems related to allergies and asthma. According to one study, “Allergens associated with dust mites (DM) and cockroaches (CR) are probably important in both onset and worsening of asthma symptoms for children who are chronically exposed to these agents. Young children spend a great deal of time on or near the floor where these allergens are concentrated in dust. Of children (2–10 years of age) living in metropolitan Washington, DC, 60% were found to be sensitive to CR and 72% were allergic to DM.”(9)
- Other mosquito-borne diseases currently endemic in the United States are Western equine encephalitis, Eastern equine encephalitis, St. Louis encephalitis, and LaCrosse virus. As noted, malaria, yellow fever, and dengue have been endemic in the past. In addition, mosquitoes transmit canine heartworms.(10)
Role of Pesticides in Promoting Health throughout History
Pesticides have proven critical in protecting public health:
- In 1966, St. Louis encephalitis (SLE), a mosquito-transmitted form of viral encephalitis, broke out in Dallas. In the space of a few weeks, mosquitoes infected up to 690 people. Dallas then aerially sprayed 475,000 acres with the pesticide malathion. The mosquito populations and the number of new SLE cases dropped dramatically. As the National Academy of Sciences (NAS) committee stated, “The economic and public health consequences would certainly have been greater had pesticides not been available.”(11)
- In 1914, when few pesticides were available, there were 600,000 cases of malaria in the United States. By 1995, when pesticides had long been a staple of public health control, the number of annual cases had shrunk to 1,167.(12)
- In 1995, dengue spread to the Mexico-Texas border. On the Mexican side of the border, where pesticides were largely not available, approximately 4,700 individuals contracted dengue. On the Texas side, where public health officials applied pesticides (and where more people have screened homes), there were only 29 cases. Only seven of the Texas cases occurred among individuals who had no history of travel outside the state.(13)
Freedom to Develop and Use Pesticides Is Key to Disease Control
Numerous experts in the field of vector control fear that government regulation jeopardizes public health by reducing the development of and access to much needed pesticides. Consider some observations from the scientific community and vector control experts:
- In 1992, an NAS report warned: “A growing problem in controlling vector-borne diseases is the diminishing supply of effective pesticides.” Because all pesticides must go through an onerous registration process at the U.S. Environmental Protection Agency (EPA), “some manufacturers have chosen not to reregister their products because of the expenses of gathering safety data. Partly as a result, many effective pesticides over the past 40 years to control agricultural pests and vectors of human disease are no longer available.”(14)
- The NAS report noted, “The potential for vector-borne disease to emerge in the United States still exists … [and] any reduction in vector control efforts is likely to be followed by a resurgence of the vector population. For a disease agent that is known or suspected to be transmitted by an arthropod vector, efforts to control the vector can be crucial in containing or halting an outbreak.”(15)
- The NAS report continued, “The primary goal at the onset of mosquito-borne disease epidemics is to eliminate the infective mosquitoes as quickly as possible. Transmission can only be stopped by the effective application of a pesticide that kills adult mosquitoes.”(16)
Issues of Safety: Pesticides versus Alternatives
Environmental activists suggest that pesticide risks are too high and that there are “more natural” means to control pests. However, the risks of disease are far greater than the risks of pesticides, and alternative controls are not nearly as effective:
- Activists provide no scientifically validated information documenting deaths or illnesses related to proper application of pesticides. In contrast, there are millions of documented deaths and illnesses related to vector-borne diseases.(17)
- Despite what activists say about the risks associated with pesticides, the EPA has studied these chemicals extensively and determined them to be safe under even the most severe exposure assumptions.

- Environmentalists claim that pesticides are so toxic they lead to wide-scale killing of wildlife, particularly birds. Accordingly, they think that pesticides should be eliminated. Although we should continue to study to find ways to reduce the impacts of pesticides on wildlife, we should not neglect the fact that wildlife is also at considerable risk from the vector-borne diseases that the pesticides control.(18)
- It appears that wildlife may be at greater risk from vector-borne diseases than from pesticides. In fact, the data indicate that the number of bird deaths related to West Nile and other diseases greatly outnumber the number related to pesticides.(19)
- In addition, environmentalists claimed that pesticide spraying led to a massive lobster die-off on Long Island in 1999. However, these claims have been shown to be unlikely according to data and studies conducted on the topic.(20)
- Electronic repellers, citronella plants, bug zappers, bats, and purple martins are not effective in controlling or repelling mosquitoes. Wayne J. Crans, research professor of entomology at Rutgers University, explains that these items and actors have limited value in actually controlling the targeted pests, and many manufacturers of such products simply take advantage of consumers by overselling the effectiveness of these products.(21)
Endnotes:
(1) Andrew A. Spielman and Michael D’Antonio, Mosquito: A Natural History of Our Most Persistent and Deadly Foe (New York: Hyperion, 2001), 61.
(2) In fact, one of the fundamental reasons for the establishment of the Centers for Disease Control and Prevention in 1945 was the eradication of endemic malaria in the United States. Happily, that goal was achieved.
(3) Ricardo Alonso-Zaldivar, “Dengue Fever is Not Quite Dead,” Los Angeles Times, January 14, 2008.
(4) Researchers believe that although Lyme disease was only recently identified (1975), the disease has been around for about 100 years, National Institute of Allergy and Infectious Disease, Lyme Disease: The Facts, the Challenge, NIH Pub. 98-3193 (Bethesda, MD: National Institutes of Health, 1998).
(5) Paul Reiter, “Global Warming and Vector-Borne Disease: Is Warmer Sicker?” Cooler Heads Coalition Briefing, Competitive Enterprise Institute, Washington, DC, July 28, 1998.
(6) World Health Organization, “Malaria,” Fact Sheet 94, World Health Organization, Geneva, 2007.
(7) Kathleen A. Orloski, Edward B. Hayes, Grant L. Campbell, and David T. Dennis, “Surveillance for Lyme Disease: United States, 1992–1998,” Morbidity and Mortality Weekly Report 49, no. SS03 (2000): 1–11.
(8) Centers for Disease control and Prevention, Division of Vector-Borne Diseases, “West Nile Virus: Statistics, Surveillance, and Control,” website paged last modified, August 9, 2011, accessed February 9, 2012.
(9) Floyd J. Malveauz and Sheryl A. Fletcher-Vincent, “Environmental Factors of Childhood Asthma in Urban Centers,” Environmental Health Perspectives 103, Suppl. 6 (1995): 59.
(10) P. G. Koehler and F. M. Oi, “Mosquitoes and Other Biting Flies,” Entomology and Nematology Department, Florida Cooperative Extension Service, Institute of Food and Agricultural Sciences, University of Florida, Gainesville, FL, 2003.
(11) Joshua Lederberg, Robert E. Shope, and Stanley C. Oaks Jr., eds., Emerging Infections: Microbial Threats to Health in the United States (Washington, DC: National Academies Press, 1992), 166.
(12) Holly Ann Williams, Jacqueline Roberts, S. Patrick Kachur, Ann M. Barber, Lawrence M. Barat, Peter B. Bloland, Trenton K. Ruebush, and Elizabeth B. Wolfe, “Malaria Surveillance—United States, 1995,” Morbidity and Mortality Weekly Report 48, no. SS-1 (1999): 1–21.
(13) Centers for Disease Control and Prevention, “Dengue Fever at the U.S.-Mexico Border, 1995–1996,” Morbidity and Mortality Weekly Report 45, no. 39 (1996): 841–44. >
(14) Lederberg, Shope, and Oaks, Emerging Infections, 160.
(15) Ibid., 160–61.
(16) Ibid., 166.
(17) Angela Logomasini, Pesticides and the West Nile Virus: An Examination of Environmentalist Claims, Competitive Enterprise Institute, Washington, DC, 2005, http://www.cei.org/pdf/3893.pdf.
(18) “West Nile Virus Threatens Backyard Birds,” Science Daily, May 17, 2007.
(19) Logomasini, Pesticides and the West Nile Virus.
(20) Ibid.
(21) Wayne Crans, “Products and Promotions That Have Limited Value for Mosquito Control,” Department of Entomology, Rutgers University, New Brunswick, NJ.
Last updated: February 10, 2012. The original text for this article was drawn from Angela Logomasini and Jennifer Zambone, “Pesticides and Public Health,” in Environmental Source, eds., Angela Logomasini, Ph.D. and David Riggs, Ph.D., Competitive Enterprise Institute, 2002 (1st ed.), 2008 (2nd ed.).

